Internship learning experience
Name:Rishitha Rao.K
UNIT DUTY:
Case 1:
35 year old female with Diminision of vision of right eye since morning 3am and Headache since 2 days
https://rishitharaok.blogspot.com/2023/05/35-female-with-diminision-of-vision-in.html
1)She also has RAPD grade 3.
https://eyewiki.aao.org/Reverse_Relative_Afferent_Pupillary_Defect_(RAPD)
Conditions Leading to a RAPD
Occur in lesions affection the visual pathway in front of the lateral geniculate body
Lesions of the Anterior Optic Pathway
Lesions of the optic nerve regardless of the cause of optic neuropathy (e.g., optic neuritis, glaucoma, compression, infection etc.)
Lesions of the optic chiasm
Lesions of the optic tract
Lesions of the pretectum
Lesions of the Retina/Posterior Segment
Large retinal detachments
Ischemia (e.g., ischemic central retinal vein occlusion or central retinal artery occlusion)
Dense macular lesions (chorioretinal scar)
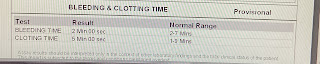
2) If it's retinal vein occlusion?Why has she developed it?
May be due to a bleeding disorder
3) About migraine and retinal vascular occlusion mechanisms.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987472/
Migraine is a complex neurological disorder that is characterized by recurrent headaches that are often accompanied by visual disturbances, nausea, and sensitivity to light and sound. While the exact mechanisms that underlie migraine are not fully understood, there is evidence to suggest that changes in blood flow and vascular reactivity may play a role.
One proposed mechanism is that migraine attacks may be triggered by a decrease in blood flow to the brain, which can cause a cascade of events leading to a release of chemicals that cause inflammation and pain. This decrease in blood flow may be due to constriction of blood vessels in the brain, followed by a rebound dilation of blood vessels that causes the throbbing pain commonly associated with migraine.
*Several studies have also suggested a link between migraine and retinal vascular changes. For example, a study published in the journal Ophthalmology found that individuals with a history of migraine were more likely to have retinal vascular changes, such as increased tortuosity and focal narrowing of retinal arterioles, compared to individuals without a history of migraine. These changes were more pronounced in individuals with a history of migraine with aura, suggesting that aura may be a marker of increased susceptibility to retinal vascular changes.
*
2. Retinal vascular occlusion,
on the other hand, is a condition where a blockage occurs in one of the retinal blood vessels, leading to damage and loss of vision in the affected area of the retina. There are two main types of retinal vascular occlusion: central retinal artery occlusion (CRAO) and central retinal vein occlusion (CRVO).
CRAO occurs when there is a sudden blockage in the central retinal artery, which supplies blood to the retina. This can lead to rapid and severe vision loss, and is often caused by emboli (clots) that originate from other parts of the body. CRVO, on the other hand, occurs when there is a blockage in the central retinal vein, which can cause swelling and bleeding in the retina. This can lead to slower and more gradual vision loss, and is often associated with systemic conditions such as hypertension, diabetes, and hyperlipidemia.
The mechanisms of retinal vascular occlusion are complex and can vary depending on the underlying cause. In general, however, it is thought that a combination of factors such
as inflammation, blood hypercoagulability, and hemodynamic changes may contribute to the development of retinal vascular occlusion. For example, studies have shown that patients with CRVO have higher levels of inflammation markers in their blood, suggesting that inflammation may play a role in the pathogenesis of the disease. Additionally, other studies have suggested that blood hypercoagulability and increased blood viscosity may contribute to the development of retinal vascular occlusion.
Overall, while the mechanisms of migraine and retinal vascular occlusion are still being studied, there is evidence to suggest that changes in blood flow and vascular reactivity may play a role in both conditions.
4) Managing migraine related retinal ischemia
Migraine-related retinal ischemia is a rare but serious complication of migraine headaches. It occurs when there is a temporary loss of blood flow to the retina, which can result in vision loss or even blindness if not managed promptly.
The management of migraine-related retinal ischemia typically involves both treating the underlying migraine disorder and addressing the ischemic event itself.
Here are some potential approaches to managing migraine-related retinal ischemia:
Medications: Medications used to treat migraines, such as triptans, may also be effective in reducing the risk of retinal ischemia. Other medications that may be used include aspirin, anticoagulants, and vasodilators.
Lifestyle changes: Adopting a healthy lifestyle can help reduce the risk of migraine-related retinal ischemia. This may include getting regular exercise, maintaining a healthy weight, eating a nutritious diet, avoiding triggers that may cause migraines, and managing stress.
. These tests may include an OCT (optical coherence tomography), FA (fluorescein angiography), or other imaging studies.
Surgery: In some cases, surgery may be necessary to address retinal ischemia. This may involve removing a blood clot, repairing a damaged blood vessel, or performing other procedures to restore blood flow to the affected area.
Follow-up care: It is important to have regular follow-up care with your healthcare provider if you have experienced retinal ischemia related to migraines. Your provider may recommend ongoing treatment or monitoring to help prevent future episodes and manage any long-term effects of the condition.
Overall, managing migraine-related retinal ischemia requires a comprehensive approach that addresses both the underlying migraine disorder and the ischemic event itself. With prompt and appropriate treatment, most people with this condition are able to recover their vision and avoid long-term complications.
Case 2:
37 years female with Pain of the left lower limb since 2 months
https://rishitharaok.blogspot.com/2023/05/37-f-pain-in-left-lower-limb-since-2.html
1)Avascular necrosis of femur as a complication of chronic steroid usage
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2784583/
Amongst the non-traumatic causes of avascular necrosis of the femur, patients of SLE who are treated with corticosteroids have been reported to have a high relative risk of developing avascular necrosis with a reported frequency of 5-40%.16
The first patient of pemphigus (described by Pietrogrande and Mastronmarino) who developed hip destruction due to corticosteroid therapy was a woman who developed avascular necrosis after four years of therapy with 100 mg cortisone acetate daily followed by a report of three cases with pemphigus developing avascular necrosis of femur.17
The duration of steroid treatment, the total cumulative dose and the highest daily dose of steroids have been implicated as important factors in the development of avascular necrosis. The incidence of males with osteoporosis is less as compared to females whether the patient is on long-term steroid
2) But was this last three month disability due to her AVN or polymyositis?
3)What are the sequence of events causally associating steroid usage and manifestation of AVN?
Case 3:
52 year old male with Pain abdomen since 3 days and 1 episode of vomiting ( 2 days back )
https://rishitharaok.blogspot.com/2023/05/52-male-acute-on-chronic-pancreatitis.html
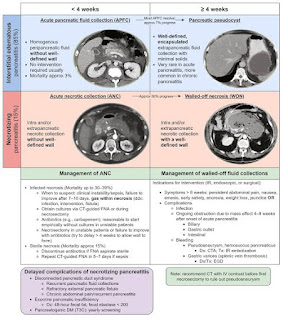
1)Why are we calling this interstitial pancreatitis?
According to the Atlanta classification, acute pancreatitis can be divided into two broad categories:
Interstitial edematous acute pancreatitis, which is characterized by acute inflammation of the pancreatic parenchyma and peripancreatic tissues, but without recognizable tissue necrosis.
Necrotizing acute pancreatitis, which is characterized by inflammation associated with pancreatic parenchymal necrosis and/or peripancreatic necrosis.
https://www.uptodate.com/contents/management-of-acute-pancreatitis#H106843438
Case 4:
80 year male with c/o hematuria since 1 week.
https://rishitharaok.blogspot.com/2023/05/80-m-with-tingling-and-numbness-of-both.html
Case 5:
30 male with pain over epigastric region since 1 day.
https://rishitharaok.blogspot.com/2023/05/30-m-with-epigastric-pain.html
PROCEDURES:
Ascitic tap on 40 year old male under the guidance of Dr.Lohith
Foleys catheterization under guidance of Dr.Narsimha
Ryles tube under guidance of Dr.Vivek
Assisted central line under guidance of Dr.venkat sai
ICU/AMC DUTY:
Taken ABG of all ICU patients
Did suction from tracheostomy tube
CPR for 70 year male
Assisted lumbar puncture procedure for 50 year male under guidance of Dr.Harika
NEPHRO DUTY:
Assisted central line under guidance of Dr.Venkat sai
Assisted in dialysis
Learned about blood transfusions
WARD DUTY:
Placed cannulas and sent investigations for ward patients
Helped my friends create PaJr groups and updated soap notes
Learned CNS examination of 50 year male with help of Dr.Himaja
PSYCHIATRY:
Learned history taking
Attended DAC rounds
Learned how to approach psychiatry patients
Seen alcohol dependence, obsessive compulsive disorder, schizophrenia cases.

Comments
Post a Comment